THE GREAT NHS GAMBLE: Doctor talks about life on the front line


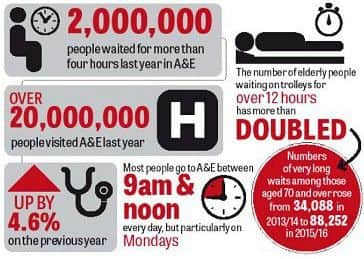
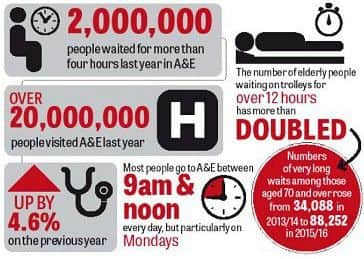
An analysis of documents drawn up to remodel the health service in England shows that 24 casualty units from Durham to Somerset have been marked for potential closure despite record demand for A&Es and serious overcrowding across the country as the NHS goes through its most severe winter crisis since records began. Last month produced the worst performance for A&E waits in 13 years. Staff are struggling to cope with the pressure.
Here Dr Sophie Gough writes about life as an A&E doctor ...
Advertisement
Hide AdAdvertisement
Hide AdDr Sophie Gough is clinical director and consultant in emergency medicine at Queen Alexandra Hospital in Cosham, Portsmouth. But she could be talking about any A&E department in the country.

Writing for Johnson Press, she has given an insight into a typical shift at the busy A&E department and the difficulties medics face.
It comes as dozens of accident and emergency units are facing closure or being downgraded in a far-reaching overhaul of urgent care which senior doctors warn would have “disastrous” consequences for the NHS.
An analysis of documents drawn up to remodel the health service in England shows that 24 casualty units from Durham to Somerset have been marked for potential closure despite record demand for A&Es and serious overcrowding across the country as the NHS goes through its most severe winter crisis in more than a decade. Last month produced the worst A&E performance for A&E waits in 13 years.
Advertisement
Hide AdAdvertisement
Hide AdNHS bosses who have drawn up the changes as part of efforts to plug a £22bn hole in the health service budget by 2021, insist that concentration of specialist urgent services could save lives and there are no plans for a ‘significant’ reduction in the existing number of 175 emergency units.

QA’s emergency department (ED) is not one of those at risk but does face substantial pressures.
‘One of our biggest challenges is flow into the hospital and patients waiting for admission,’ writes mother-of-two Dr Gough.
‘This is a national problem, with many medically fit patients waiting for packages of care.
Advertisement
Hide AdAdvertisement
Hide Ad‘This can mean there are delays in discharging patients from hospital, which leads to long waits in the emergency department.
‘We saw approximately 130,000 patients in the ED last year, over 300 per day. There are approximately 120 emergency admissions to the hospital per day.
‘We do sometimes get the occasional disruptive patient, which may because they are unwell, but also when they are under the influence of drugs or alcohol.
‘This is worse in the evenings or weekends, but doesn’t account for many patients.
Advertisement
Hide AdAdvertisement
Hide Ad‘When demand on the service outweighs the discharges from the hospital, the pressures are felt in ED.
‘When the GP has no more appointments, you get offered an appointment for another day.
‘ED is open all the time, we can’t close our doors. When it becomes busy the ED team works hard, with all members of staff helping to see patients.
‘Even if the department is full, it is still important to see new patients as quickly as possible.
Advertisement
Hide AdAdvertisement
Hide Ad‘There is pressure on all emergency departments in England and here is no different. There is huge pressure on the NHS and this is felt in the Emergency Department.
‘Primary care (GP) is also under huge amounts of pressure which also affects the numbers of patients presenting to the ED.
‘Over the past eight years as a consultant and 19 years as a doctor, I have noticed a societal change. Patients are less willing to wait, and want ‘instant’ health care.
‘As a society we need to take responsibility for disease prevention – smoking cessation, reduction in alcohol consumption, weight loss and increasing our activity levels. If we don’t we are storing up healthcare problems for the future.
Advertisement
Hide AdAdvertisement
Hide Ad‘In the age of social media people (all age groups) want instant health care. Patients are not willing to wait and therefore will not infrequently present to the ED. I have no way of changing your outpatient appointment or speeding up routine investigations. Emergency medicine is a fantastic speciality where I have the privilege of treating patients in an emergency.
‘I enjoy the variety, and not knowing what I will treat next.
‘It is hugely satisfying when you treat someone and save their life. It is also satisfying treating patients with non – life threatening conditions like fractures and lacerations. These conditions are important to those patients.’
Dr Sophie Gough writes: ‘A typical shift is busy and varied, treating all patients of all ages and conditions that present to the department.
Advertisement
Hide AdAdvertisement
Hide Ad‘This will be reviewing new patients presenting to the department, as well as giving on going care to patients that are in the department waiting for admission.
‘As a senior doctor I also support and help junior doctors and nurse practitioners with decision making and care for the patients they see and we provide medical advice to the walk in centres.
‘At the beginning of any shift there is a comprehensive handover from the out-going team to the new team. We handover any outstanding investigations or treatments, as well as identify patients who are unwell that require a consultant review.
‘We have a computerised system that patients have all their observations (pulse, blood pressure, respiratory rate, level of consciousness, oxygen levels and if they are in pain) are recorded on.
Advertisement
Hide AdAdvertisement
Hide Ad‘Based on these figures the system identifies patients that are unwell, highlighting this to the clinician and prompting a review.
‘Once this handover is complete, my priority is to review the unwell patients.
‘Next I will review patients that could be safely discharged home. This will create capacity for new patients. At the beginning of the day the department is often nearing full capacity.’
‘I work in a fantastic team of doctors, nurses, receptionist, admin staff, porters, cleaners, managers and volunteers.
Advertisement
Hide AdAdvertisement
Hide Ad‘All of which are essential for the running of the department.
‘I am one of 16 full or part-time consultants working in the department supporting 30 junior doctors. There are 206 full or part-time nurses, with 22 nurses working during the day and 18 at night.
‘All the staff work shifts, with a consultant presence in the department for at least 16 hours a day. There is always a consultant or registrar and a senior nurse working in the department.’